76
77
Very interesting. Vaccines can induce immune responses to clear persistent viral infection. Relevance to #longCOVID?
In this WAS patient;
1) mRNA vax (but not infection) induced antibody to the Spike
2) mRNA vax ⬆️ IFN-g secreting T cells
3) Vax cleared persistent 🦠 twitter.com/Primary_Immune…
78
“COVID toes” are swollen discolored toes (and fingers) that were seen in areas with high incidence of COVID-19, but the cause is unknown. This new study by @JeffGehlhausen et al shows lack of association between covid toes and SARS-CoV-2 infection. 🧵(1/)
pnas.org/content/119/9/…
79
To help the parents navigate the COVID vaccines now approved for younger children, I collaborated with Dr. Thomas Murray @YalePediatrics @yalepedsid @ynhhealth to create this table using @BioRender for primary COVID vaccine series for different age groups.
Please share! (1/)
80
Nasal Spray Booster Keeps COVID-19 at Bay - an excellent piece by Meghan Rosen.
So grateful to @HHMINEWS for stepping up and supporting our research efforts on COVID - on acute COVID, #longCOVID pathogenesis and vaccine strategies against SARS-CoV-2 🙏🏼
hhmi.org/news/nasal-spr…
81
There are multiple hypotheses behind long COVID pathogenesis including persistent virus/viral remnants, autoimmunity, dysbiosis, virome reactivation and tissue damage. Our data will dive deep into some of these. (3/)
science.org/doi/10.1126/sc…
82
A Phase 2 clinical trial of oral camostat mesylate during early phase of COVID-19 in outpatients reduced illness course (including fatigue) and prevented loss of smell and taste!
Work of fantastic colleagues at @YaleMed. (1/)
medrxiv.org/content/10.110…
83
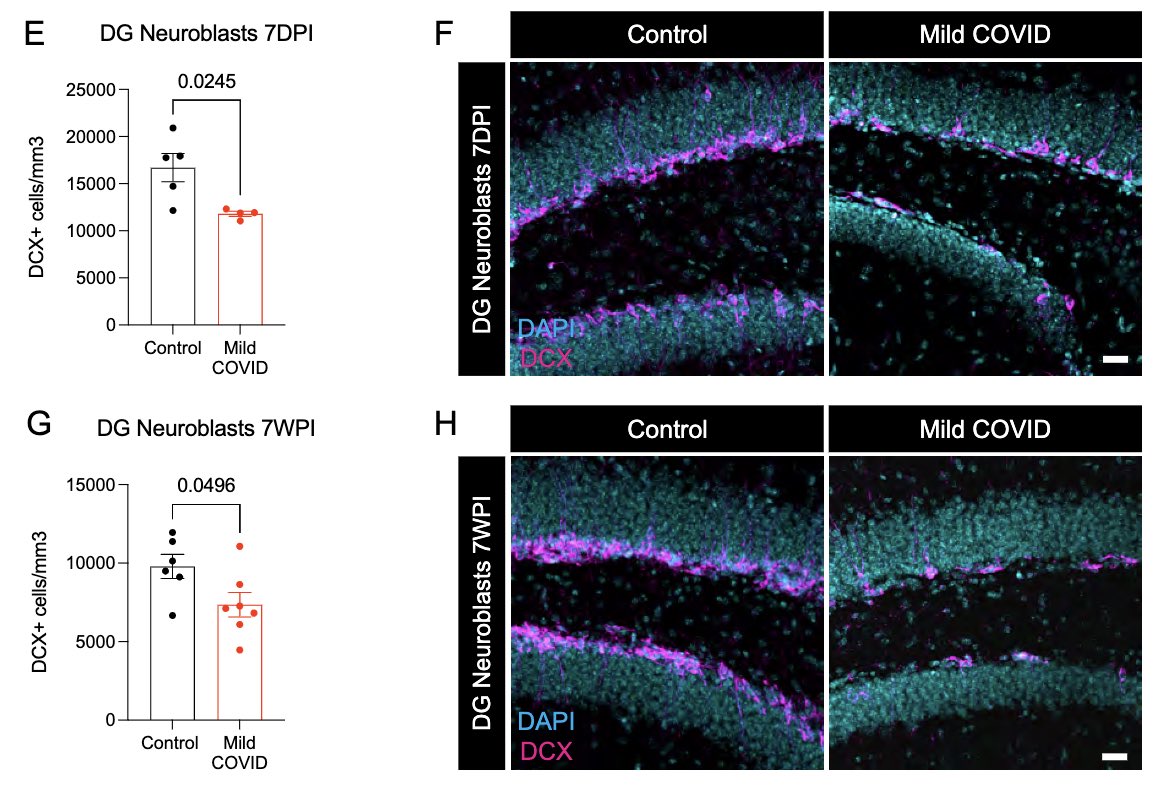
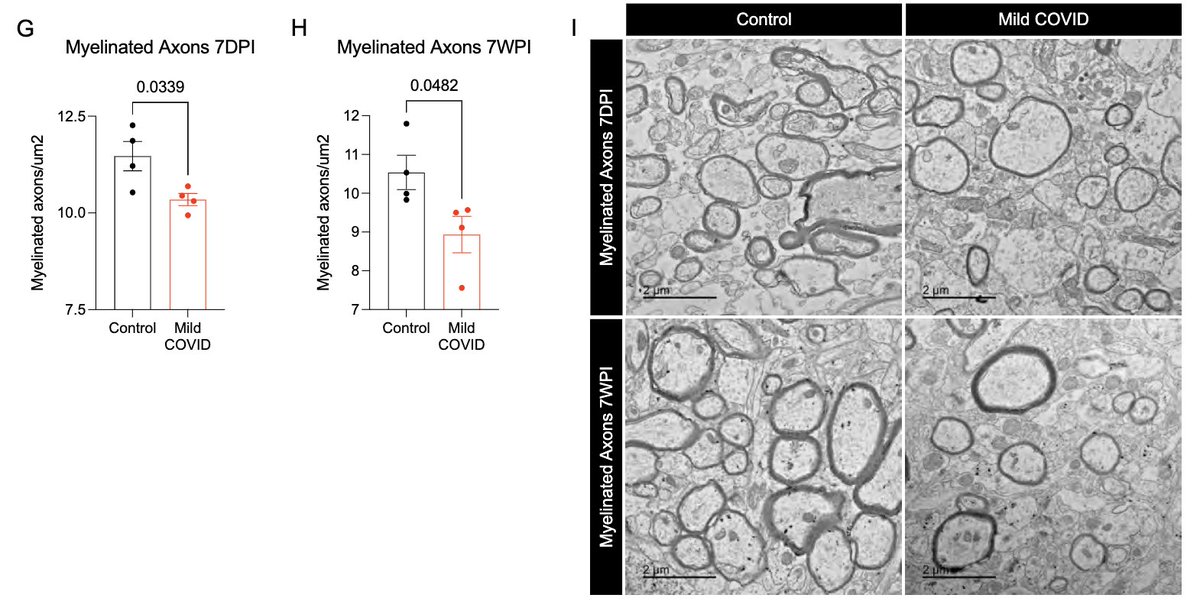
This study also opens up all kinds of questions and possibilities. For example, therapies that can 1) block inflammatory cytokines, 2) block inducers of such cytokines, or 3) reset reactive microglia can be considered for future clinical trials. Thank you for reading till end.
84
85
In #longCOVID patients, “exercise capacity was primarily limited by impaired systemic EO2 of such severity that what should have been an adequate increase in DO2 was insufficient to allow for an increase in VO2.” Via @YalePCCSM
sciencedirect.com/science/articl…
86
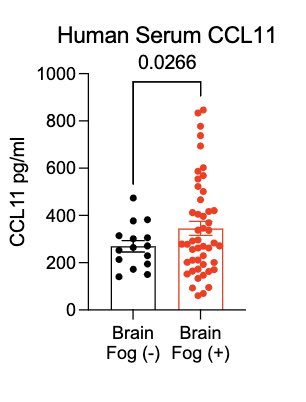
In collaboration with @PutrinoLab at @MountSinaiNYC, we found significantly elevated circulating levels of CCL11 in long COVID patients who reported brain fog vs. those who did not. Many 🙏🏼 to @wood_jamie_1 @LauraTabacof @GeneticHeartDoc #DaynaMcCarthy & the patients! (11/)
87
My lab is looking for a project manager. If you are interested in a research associate position to oversee biorepository and manage cool #longCOVID immune profiling and #neuroimmune mouse projects, please apply below 👇🏽
sjobs.brassring.com/TGnewUI/Search…
88
With millions of #longCOVID patients, it is becoming better known that even a mild infection can lead to longterm debilitating health problems. SARS-CoV-2 joins the long list of other pathogens that cause post-acute infection syndrome (PAIS). (2/)
89
90
So wonderful to see this work published! Timing is everything when it comes to immune control of COVID. Neutralizing antibody production is delayed in lethal COVID. By the brilliant @carolilucas @sneakyvirus1 & #YaleIMPACT team 💪🏼(1/n) twitter.com/NatureMedicine…
91
What an incredible honor to be invited to have lunch at the @WhiteHouse by Dr. Jill Biden in honor of Mrs. Yuko Kishida, spouse of the Prime Minister of Japan. I discussed #LongCovid, nasal vaccines, and the importance of science with powerful women 🌸
asahi.com/ajw/articles/1…
92
@cstroeckw Many thanks to you and other patient advocates, this pandemic has propelled me to investigate the pathobiology of #longCOVID, #MECFS and #longLyme 🙏🏼 If enough people do the same, we can change how society and medicine view post-acute infection syndromes.
93
Current COVID vaccines are given intramuscularly. This induces robust circulating antibodies and systemic T & B cell responses that block viral spread and disease. However, to better block infection, immunity has to be established at mucosal surfaces. (2/)
annualreviews.org/doi/10.1146/an…
94
Very important work by @PGTimmune and colleagues showing that repeated SARS-CoV-2 antigen exposure (infection and/or vaccines) does not lead to an exhausted T cell phenotype.
#GetBoosted
nature.com/articles/s4159… twitter.com/PGTimmune/stat…
95
We hope that our study will be informative to others working in the field. We need validation across cohorts. We also hope that these data will help those who are still skeptical understand that long COVID is real, and it has biological basis. Thank you for reading. (End)
96
What an honor to be featured in the latest BBC Science in Action with @michelle_monje! We discuss our latest research on how mild respiratory COVID can cause multi-lineage neural dysregulation with @PeaseRoland. Many thanks to @AndrewLuckBaker 🙏🏼
bbc.co.uk/sounds/play/w3…
97
Sincere thank you to many of you who reached out to @POTUS and @WHCOVIDResponse in support of our efforts on nasal booster vaccine 🙏🏼
I will be speaking at the White House Summit on Future of COVID-19 Vaccines on July 26.
RSVP to join via livestream: pitc.zoomgov.com/webinar/regist…
98
99
100
For example, can we target viral reservoir with antivirals and mAbs? Can we restore cortisol levels? Should therapy be targeting EBV? Would immunomodulatory therapy against inflammatory cytokines be useful? We still need to identify long COVID endotypes for treatment. (27/)