26
So grateful to receive the 2022 Johadamis ME/CFS Research Grant! In collaboration with @polybioRF @BjornBragee we will test blood & CSF samples from #MECFS patients for immune phenotypes and antibodies to various pathogens. This will inform us about potential drivers of disease. twitter.com/Tempi_Stiftung…
27
Very excited to receive the book THE LONG COVID SURVIVAL GUIDE edited by @fi_lowenstein. This book has many great insights and ‘how-to’ tips from amazing patient experts and researchers, including @PutrinoLab. Honored to contribute an afterword 🙏🏼 #MustRead #longcovid
28
Nasal booster with recombinant spike protein or spike mRNA in PACE converts systemic immunity induced by primary vaccines into mucosal immunity
⬇️ Infection
⬇️ Transmission
🚫 Disease
Prime and Spike is published today 👇🏽
@tianyangmao @BenIsraelow
science.org/doi/10.1126/sc…
29
A more general discussion and powerful testimony by #longCOVID patients can be found in this video by @KnowableMag. I share hypotheses on disease pathogenesis and discuss possible therapies. Please listen to the patients and learn more.
knowablemagazine.org/article/health…
30
For those who are interested in learning more about how COVID and #longCOVID can impact the brain, I highly recommend this video interview by @KnowableMag of @michelle_monje 👇🏽
knowablemagazine.org/article/health…
31
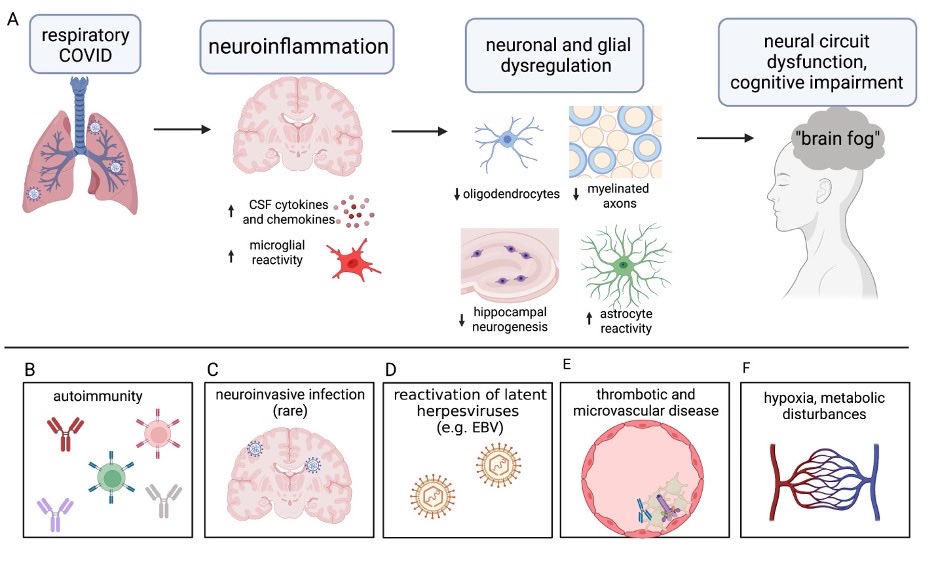
Grateful for the opportunity to coauthor this review with the incredible @michelle_monje 🙏🏼 We discuss pathobiology of #longCOVID in the central nervous system and speculate on chief mechanisms that contribute to this emerging neurological health crisis.
cell.com/neuron/fulltex…
32
新型コロナ後遺症に関する私たちの研究についてお話しを記事にしていただきました。メカニズムの解析は進んでいますが、さらなる研究と臨床試験が必要です。世界中で苦しんでいる多くの人に役立つ治療に貢献したいです。是非日経サイエンスの特集を読んで下さい👇🏽 #longCOVID
nikkei-science.com/202211_039.html
33
Very happy to see that China approved the world’s first inhaled vaccine against COVID-19. Convidecia Air is an aerosolized vaccine based on Ad5-nCoV made by Cansino.
fortune.com/2022/09/05/can…
34
I could not agree more with @EricTopol 👇🏽
While we are gaining more insights into the disease pathogenesis of #longCOVID, we also need to start well-designed randomized clinical trials now! Patients cannot wait any longer, and scientists will learn from RCTs to improve therapy. twitter.com/EricTopol/stat…
35
Here is the summary of our findings. There are many implications for diagnosis and therapy for #longCOVID. (26/)
36
We hope that our study will be informative to others working in the field. We need validation across cohorts. We also hope that these data will help those who are still skeptical understand that long COVID is real, and it has biological basis. Thank you for reading. (End)
37
For example, can we target viral reservoir with antivirals and mAbs? Can we restore cortisol levels? Should therapy be targeting EBV? Would immunomodulatory therapy against inflammatory cytokines be useful? We still need to identify long COVID endotypes for treatment. (27/)
38
39
40
41
Finally @rahuldhodapkar used machine learning and found that immune features alone can predict long COVID with efficient discriminative performance (AUC=0.96)! The most informative individual data blocks contributing to efficient separation of groups are flow and cytokine. (21/)
42
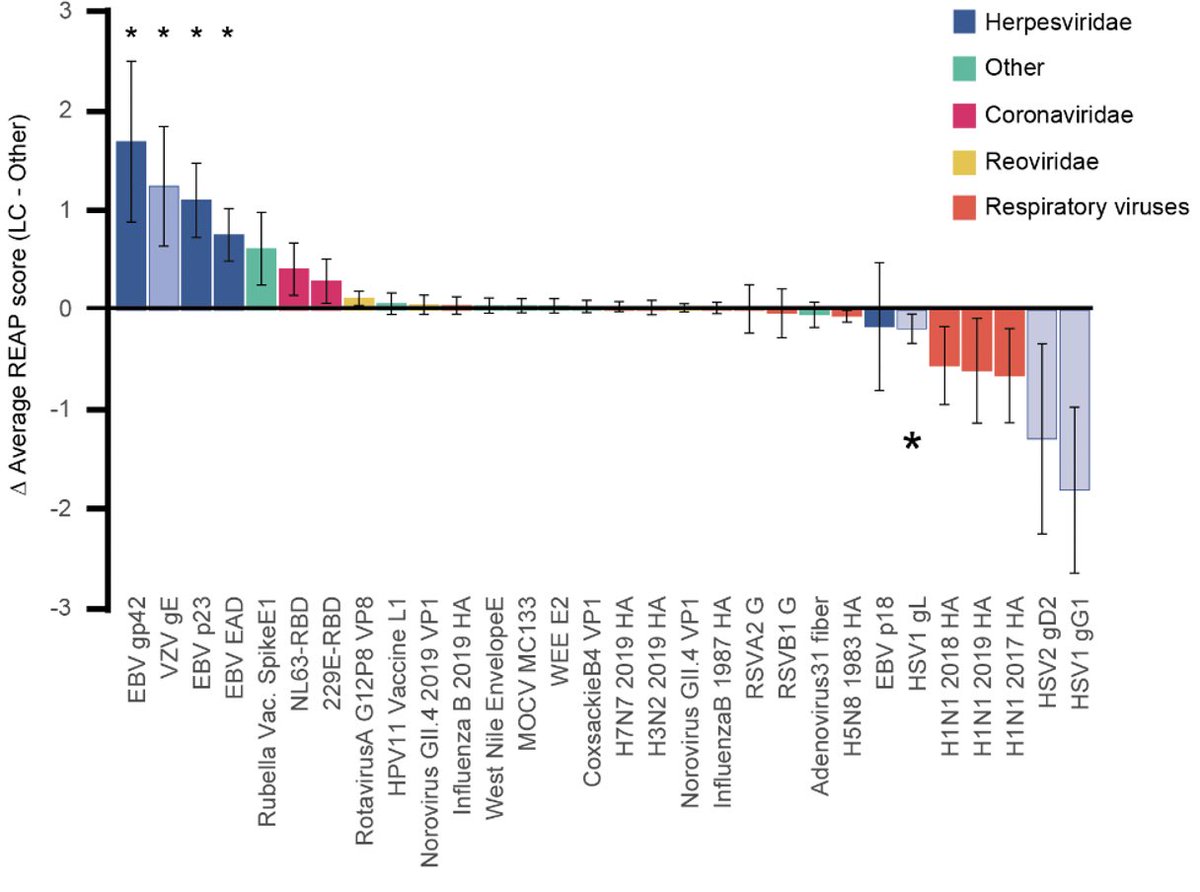
This again is consistent with the report by @SuYapeng et al, showing that EBV viremia at the time of diagnosis is one of the four predictive factors for long COVID. (Note that our study did not examine viremia but infer EBV reactivation by serology)(19/)
sciencedirect.com/science/articl…
43
The increases in antibodies to EBV and VZV antigens were also detected using independent assays like ELISA and @serimmune epitope mapping. However, seroprevalence for EBV and VZV were similar in LC and CC. These data suggest recent reactivation of EBV and VZV in LC. (18/)
44
45
46
This is so interesting, giving the report by @SuYapeng et al showing similar reduction in long haulers with respiratory viral symptoms at 2-3 months post COVID. This implies chronic hypocortisolism in long COVID. (14/)
47
48
49
50