51
Has anyone else with #longCOVID received monoclonal antibodies to SARS-CoV-2? Please share your experience. More data will help justify a clinical trial. Thank you. twitter.com/AlisaValdesRod…
52
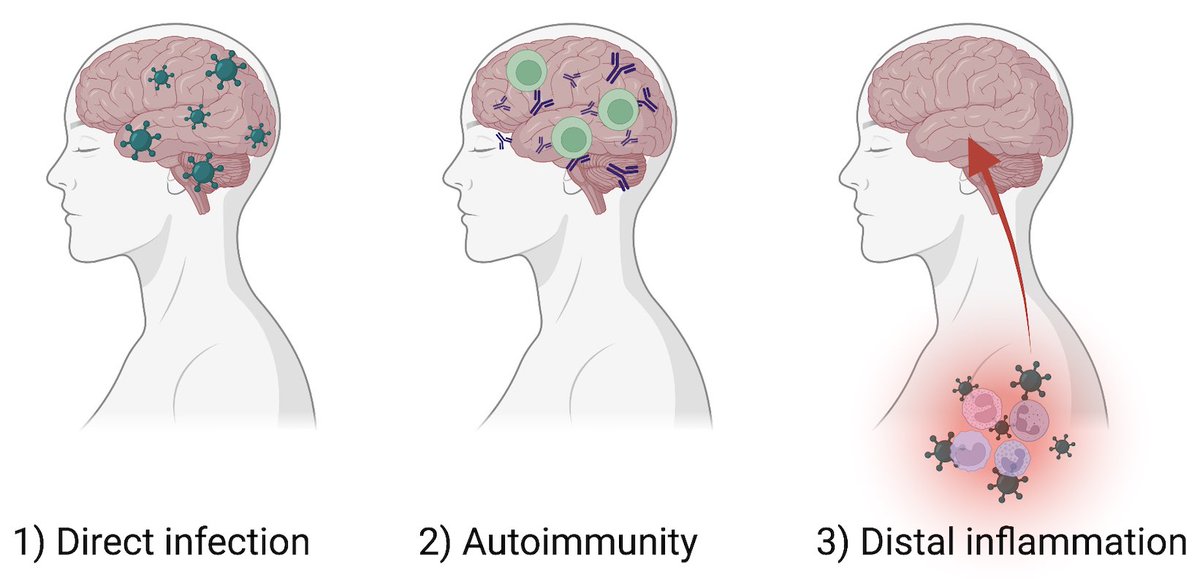
So excited to be a part of this important study led by @michelle_monje on how significant longterm neurologic damage can occur after a mild respiratory-only SARS-CoV-2 infection. My own🧵on the findings of this study with relevance to #longCovid (1/)
biorxiv.org/content/10.110…
53
54
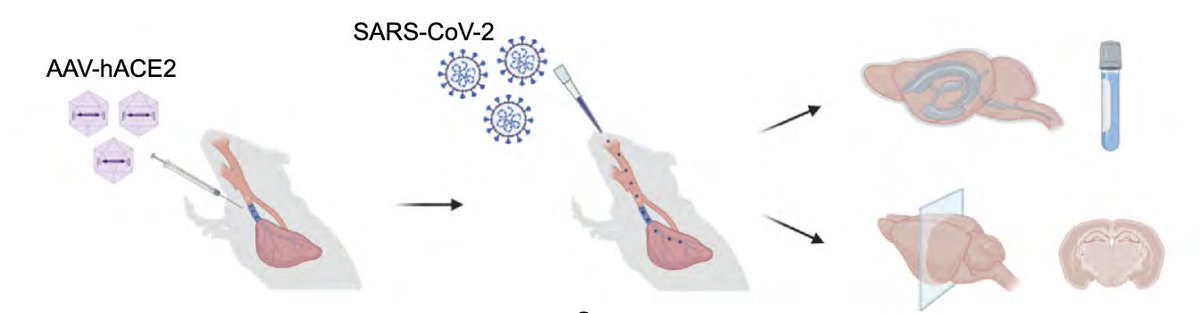
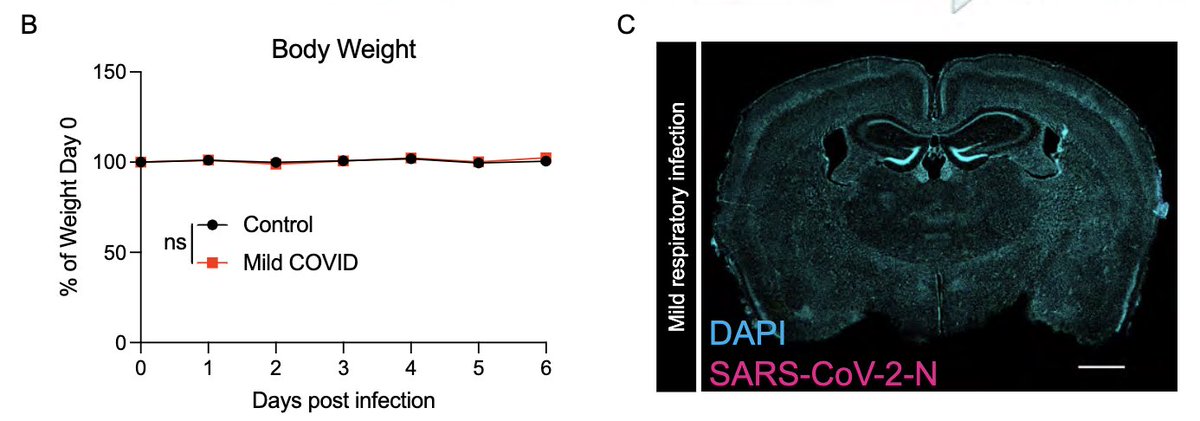
To achieve this goal, @peowenlu & @ericsongg used a mouse model developed by @BenIsraelow & @ericsongg in which we can control where the infection happens. Using AAV-hACE2 intratracheally, we can confine the SARS-CoV-2 infection only to the lungs. (3/)
rupress.org/jem/article/21…
55
56
57
58
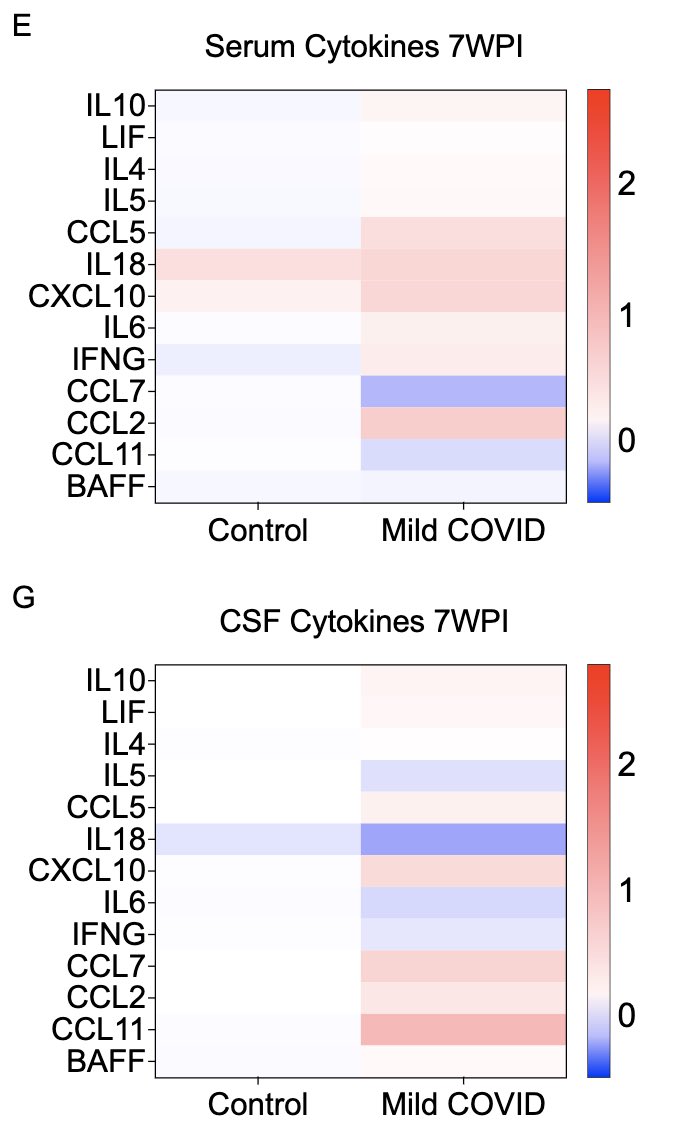
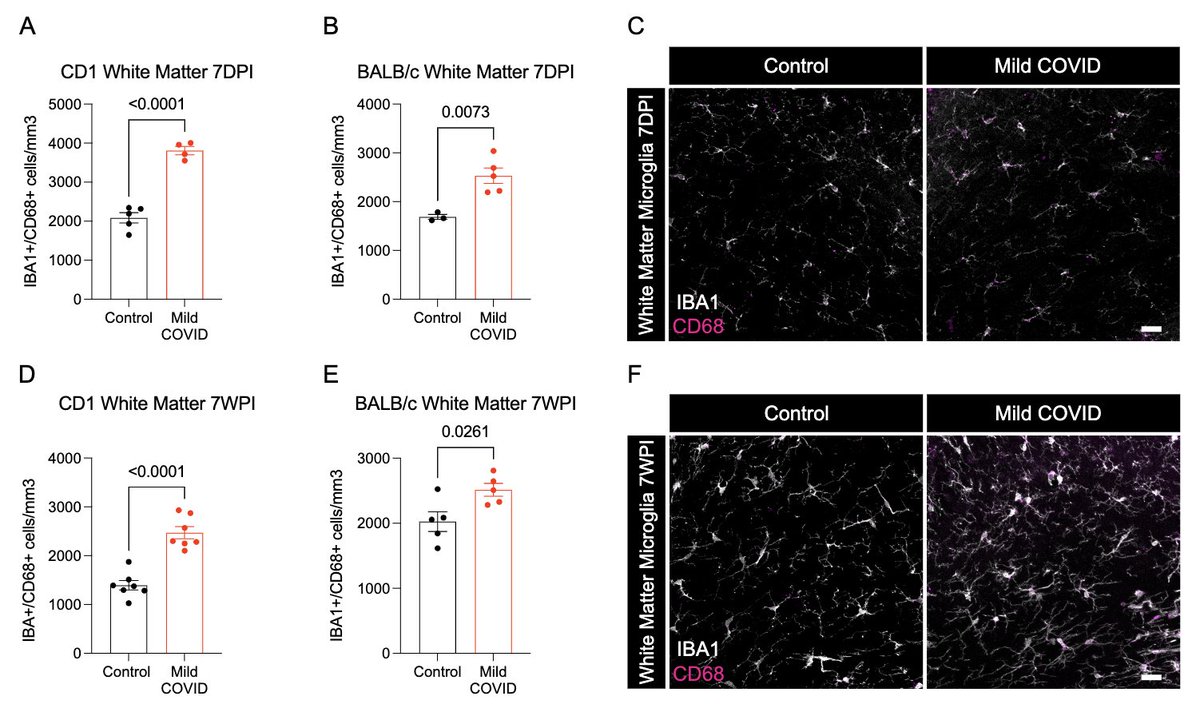
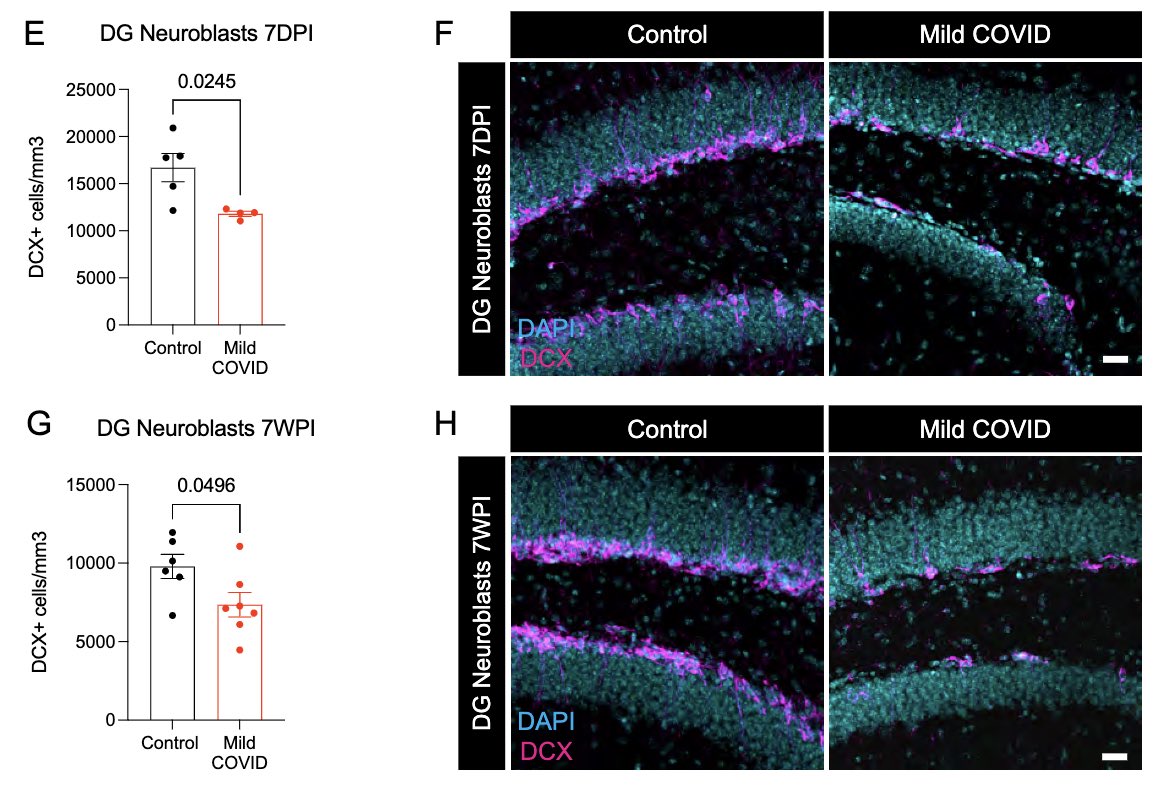
What does a respiratory-only mild COVID do to the brain? @ThisIsAnthonyFC and @AnnaGeraghty2 examined the subcortical white matter of two independent strains of mice and found consistently increased microglial reactivity at 7 days and 7 weeks post infection. (7/)
59
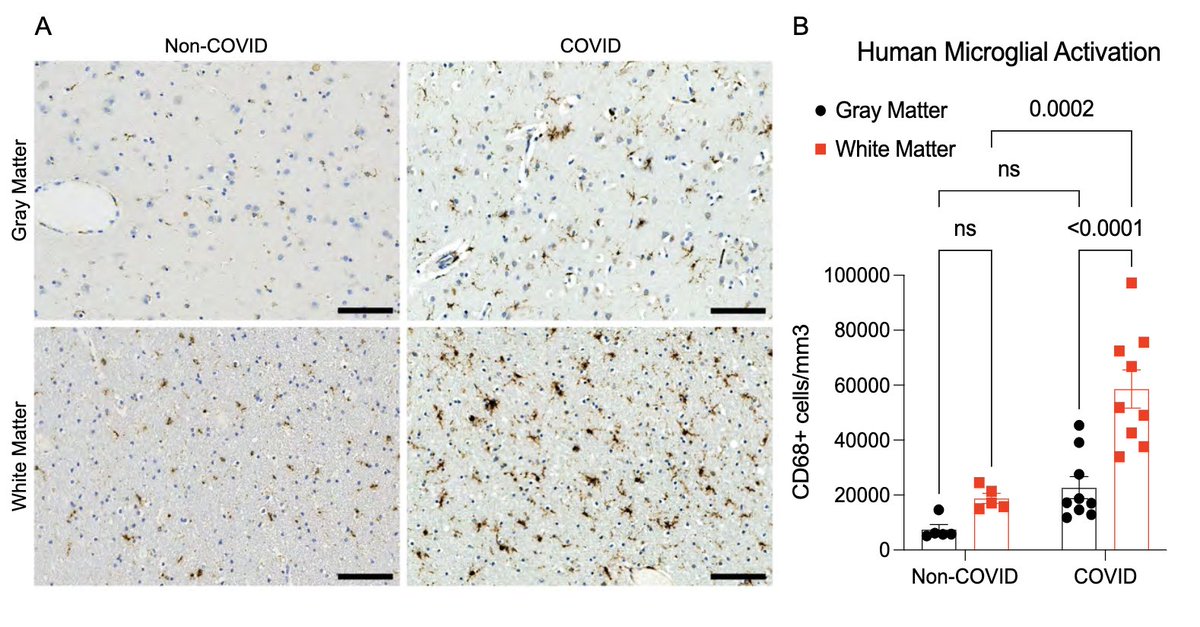
Next, with @nathavindra, autopsies from 9 individuals found to be SARS-CoV-2-positive by nasal swab PCR at the time of death were examined. Brains from those with even mild or asymptomatic SARS-CoV-2 infection had microglial reactivity in subcortical white matter. (8/)
60
61
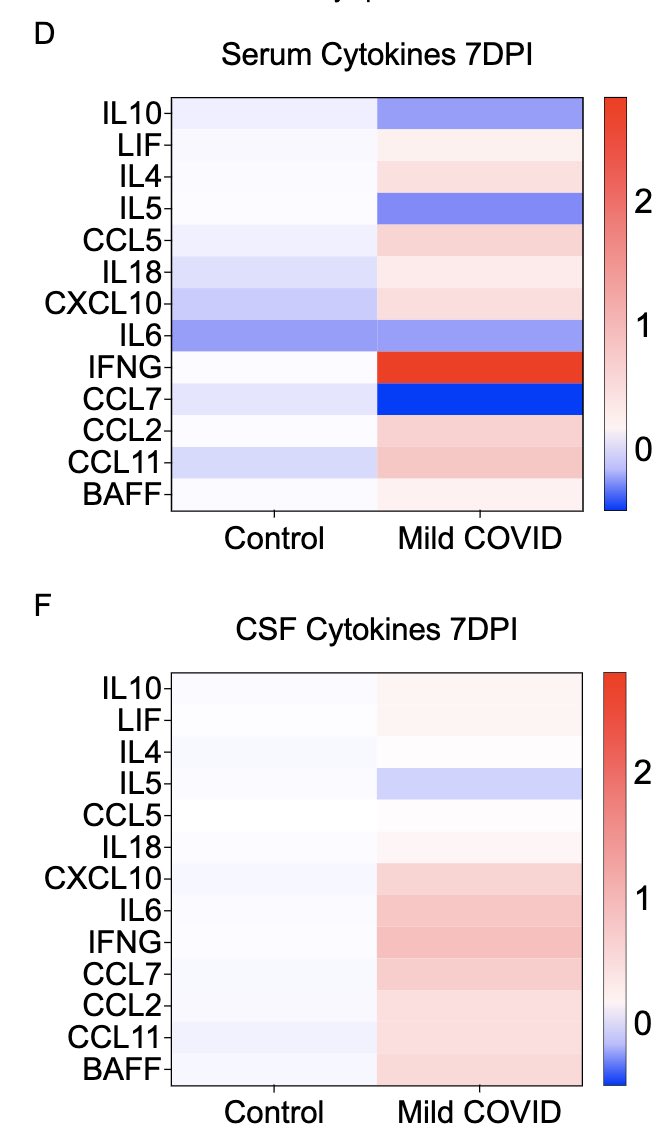
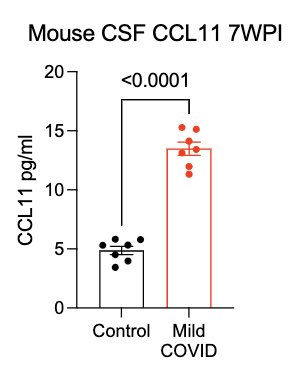
What can lead to impaired neurogenesis in hippocampus? We looked into a chemokine called CCL11 (eotaxin-1) which was shown to reduce neurogenesis (Villeda et al). In our mice, CCL11 was elevated in the CSF 7 weeks after mild respiratory infection. (10/)
pubmed.ncbi.nlm.nih.gov/21886162/
62
In collaboration with @PutrinoLab at @MountSinaiNYC, we found significantly elevated circulating levels of CCL11 in long COVID patients who reported brain fog vs. those who did not. Many 🙏🏼 to @wood_jamie_1 @LauraTabacof @GeneticHeartDoc #DaynaMcCarthy & the patients! (11/)
63
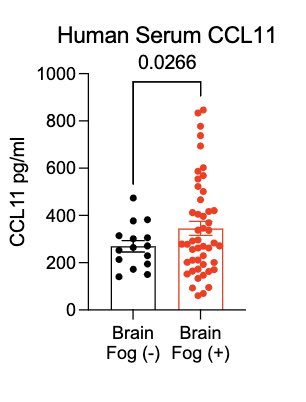
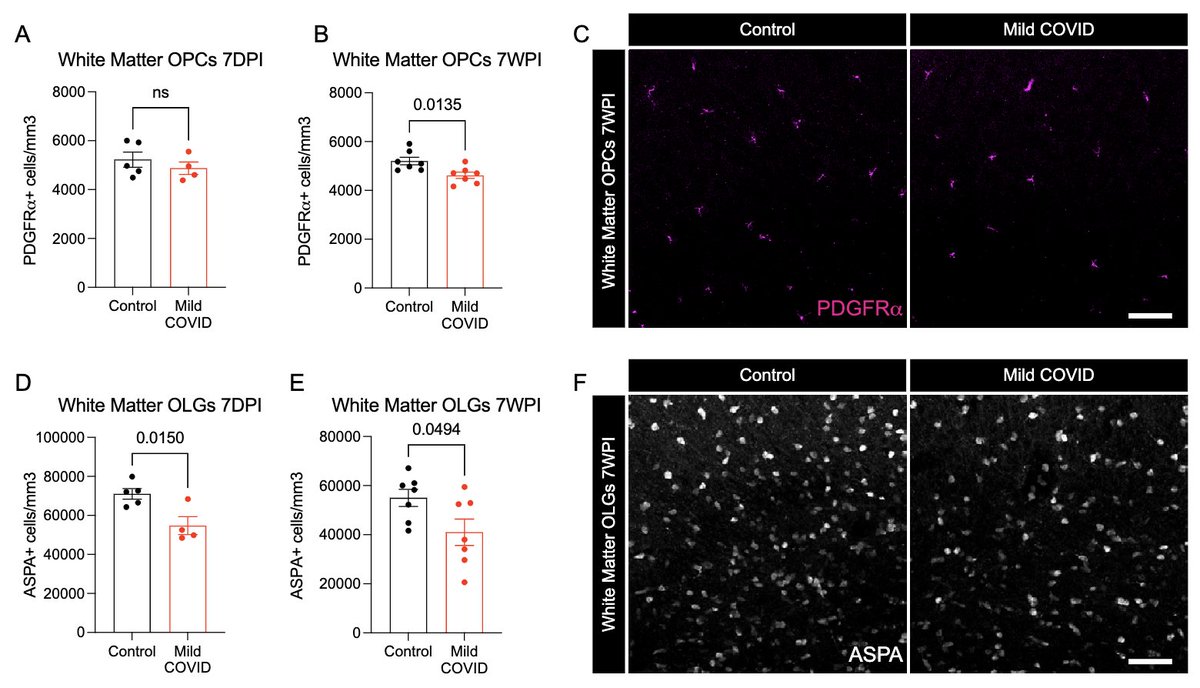
What other changes are happening in the brain of mice with mild respiratory infection? Within just 7 days of infection, we found a loss of ~1/3 of oligodendrocytes, which persisted for at least 7 weeks! Analysis by @ThisIsAnthonyFC and @AnnaGeraghty2 (12/)
64
65
This study was led and executed by my amazing colleague, @michelle_monje & her team + @PutrinoLab @MountSinaiNYC, @nathavindra et al. From our Yale team, I wish to highlight @peowenlu @ericsongg and others listed here 💪🏼 (14/)
66
In a nutshell, this study illustrates that respiratory-only mild SARS-CoV-2 infection can lead to detrimental changes in the brain, likely mediated by inflammatory factors. Similar neuropathobiology may be shared in chemo-brain, post-ICU syndrome and ME/CFS. (15/)
67
This study also opens up all kinds of questions and possibilities. For example, therapies that can 1) block inflammatory cytokines, 2) block inducers of such cytokines, or 3) reset reactive microglia can be considered for future clinical trials. Thank you for reading till end.
68
I highly recommend this very informative thread posted by @michelle_monje on this study. twitter.com/michelle_monje…
69
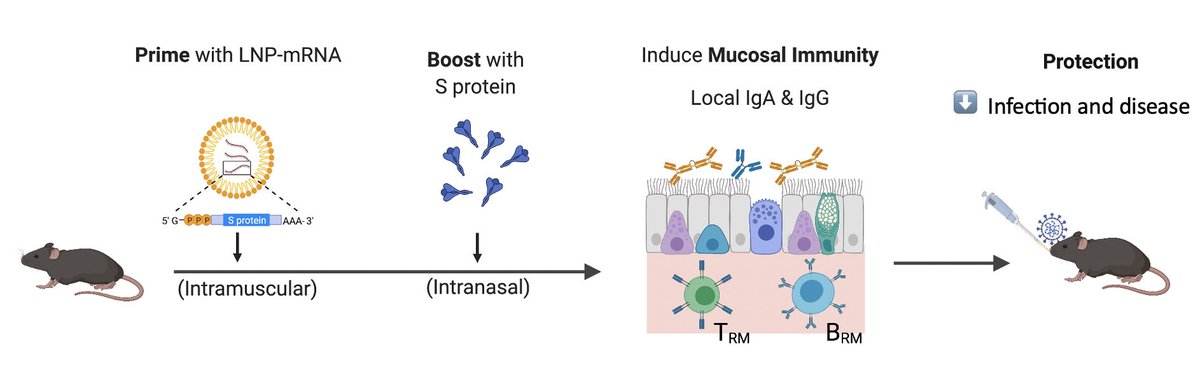
Vaccines that reduce infection & disease are needed to combat the pandemic. Here, @tianyangmao @BenIsraelow et al. describe our new mucosal booster strategy, Prime and Spike, to induce such immunity via nasal delivery of unadjuvanted spike vaccine 🧵 (1/)
biorxiv.org/content/10.110…
70
Current COVID vaccines are given intramuscularly. This induces robust circulating antibodies and systemic T & B cell responses that block viral spread and disease. However, to better block infection, immunity has to be established at mucosal surfaces. (2/)
annualreviews.org/doi/10.1146/an…
71
To elicit mucosal immunity from scratch, live attenuated vaccines are often necessary, due to the need to introduce sufficient antigen and innate immune signals needed for priming via mucosal surfaces. Live vaccines are not safe for immunocompromised. (3/)
nature.com/articles/s4157…
72
73
Omg 🤩
Our Prime and Spike 👃🏼 vaccine story is in the @RollingStone 👩🏻🔬
By @daxe with comments from @BenIsraelow
rollingstone.com/culture/cultur…
74
Nasal Spray Booster Keeps COVID-19 at Bay - an excellent piece by Meghan Rosen.
So grateful to @HHMINEWS for stepping up and supporting our research efforts on COVID - on acute COVID, #longCOVID pathogenesis and vaccine strategies against SARS-CoV-2 🙏🏼
hhmi.org/news/nasal-spr…
75
The latest summary of “How Long Covid Exhausts the Body” by @joshkellerjosh. Visual journalism at its best 👀
Happy to contribute insights with @nathavindra. Ft. @PutrinoLab @michelle_monje @microbeminded2 @Survivor_Corps @itsbodypolitic & patients.
nytimes.com/interactive/20…